More than 7 million Americans with diabetes rely on insulin. All have been affected by rapidly rising insulin costs over the past two decades.
Today a particular brand of insulin costs 8.5 times what it did fifteen years ago: $1,487 per vial in 2019, compared to $175.57 for the same size vial in 2004.
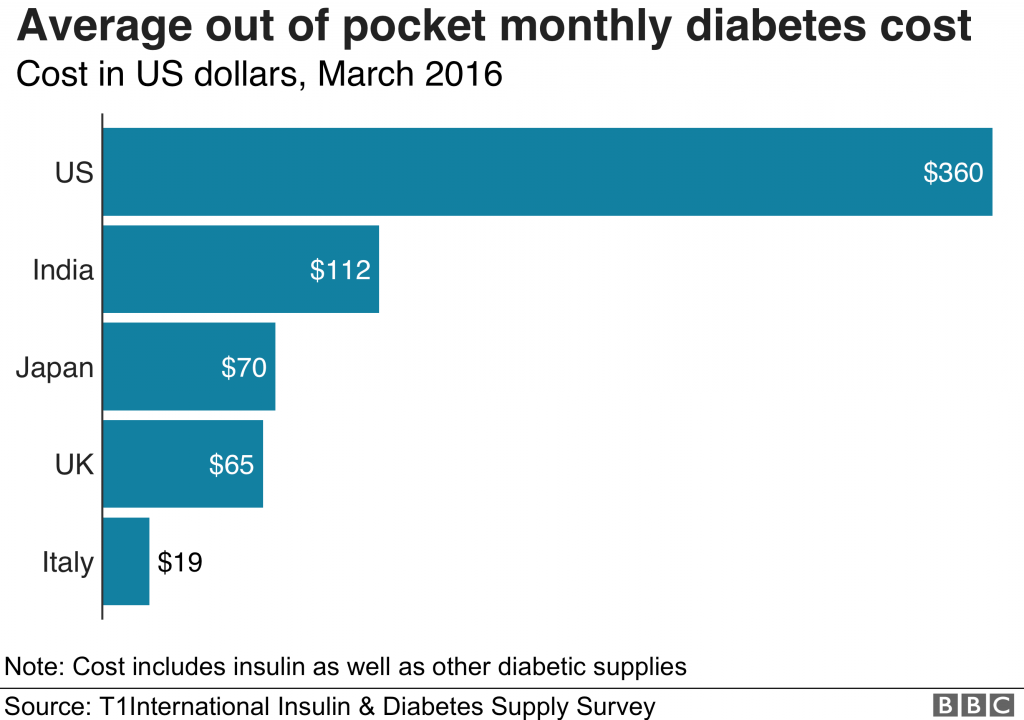
Insulin is a natural hormone that regulates glucose levels in the blood. The amount taken (and, therefore, its price) varies for each person and depends on factors like age, weight, diet and overall health. But on average, in 2016, Americans on insulin were paying $210/month, while across the pond, British residents paid only $65/month for the exact same drugs. Nowadays, the out-of-pocket expense for an uninsured, young adult male in the U.S. could be as much as $1,300/month. While insulin’s escalating cost has the biggest impact on the uninsured, under-insured and those with Medicare coverage gaps, those who are insured can also face excessively high costs. An insured, diabetic advocate reports paying $2,400 for a month’s supply of insulin.
In the best-case scenario, insulin is a significant factor in a diabetic’s budget. But for cash-strapped patients in America, the extortionate cost means living in fear, with a singular focus on how to afford the lifesaving treatment.
Many will burn through savings and be forced to raise money in GoFundMe campaigns. Others will travel thousands of miles to (technically, illegally) purchase cheaper insulin from Canada and Mexico. Perhaps most troubling is a recent study that found 1 of every 4 diabetics using insulin have rationed their use to keep costs down. Rationing and general lack of access to insulin can have harrowing health outcomes, including diabetic ketoacidosis, hospitalization and even death.
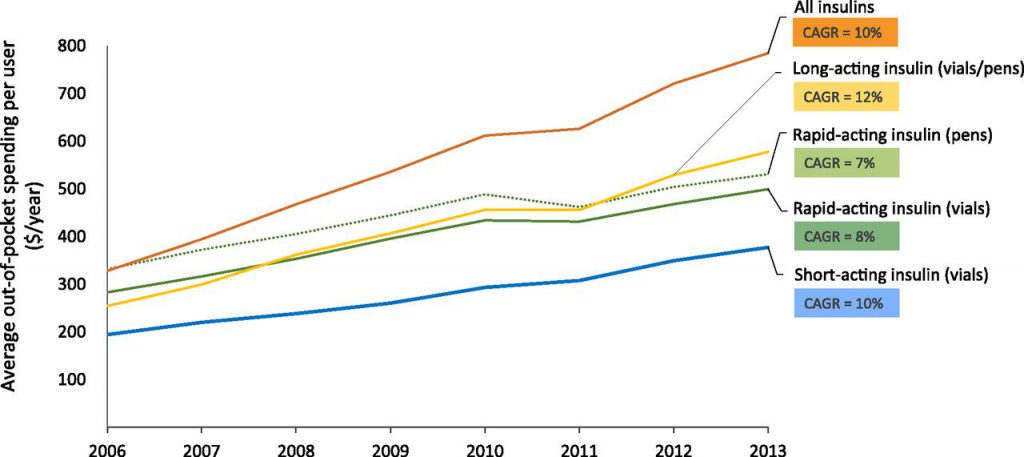
An American Diabetes Association working group found that between 2002 and 2012, insulin prices tripled. Then, more recently, the costs of insulin doubled, from approximately $2,864/year in 2012 to $5,705/year by 2016. By 2016, insulin was the leading cost driver for the more than $6,000 increase in gross health care spending for Type 1 diabetics, according to the Health Care Cost Institute (HCCI).
By 2030, 79 million people around the world will require insulin to manage Type 2 diabetes, but only 38 million will have access to it, a problem that is only exacerbated by rising costs.
Making insulin affordable could require new government regulations on pharmaceutical companies and an overhaul of the U.S. healthcare system. (That shouldn’t be too hard!) But in the meantime, there is some good news. By committing to sustainable, healthy lifestyle changes, prediabetics have the ability to avoid insulin dependency and its financial burden altogether.
In addition, many Type 2 diabetics who…
- are not yet on insulin, or
- have been advised by a physician that a healthier lifestyle could enable them to reduce or eliminate the need for insulin
…. can also avoid or reduce high insulin costs, by committing to healthier lifestyles and choices. Recent studies show us that through diet and exercise many Type 2 diabetics have the ability to gain greater control over both their health and future financial freedom.
Healthiby’s wellness rewards solution offers what could be the most financially attractive alternative to insulin that exists on the market today.
Sources of images:
- Graph showing the rising costs of insulin, titled “Average Medicare out-of-pocket spending for insulin, per user, by product category, 2006–2013” Source: USC Schaeffer Center analysis of Medicare Part D claims data.
- Graph showing international price comparison, titled “Average Out-of-Pocket Monthly Diabetes Cost” Source: T1Insulin International Diabetes Supply Survey, March 2016, https://www.bbc.com/news/world-us-canada-47491964

